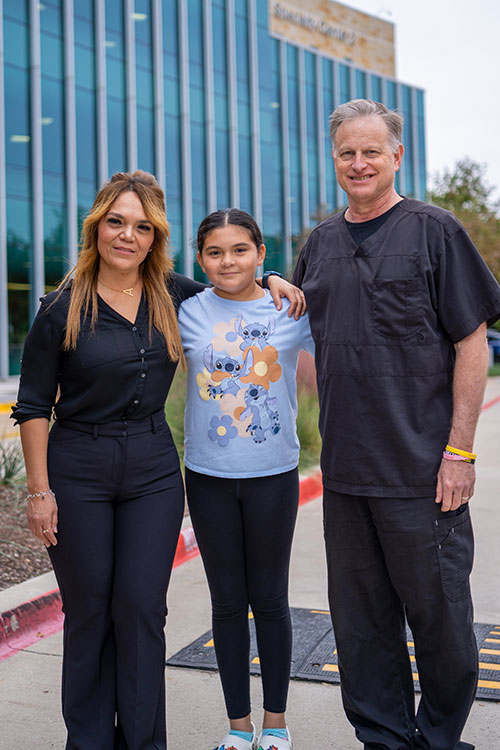
Interview by Angelica Villa. Photos provided by Children's Health.
In recognition of Mental Health Awareness Month, we are honored to host a Q&A with Dr. Andy McGarrahan, PhD, a dedicated psychologist at the Center for Pediatric Eating Disorders at Children’s Medical Center Plano and an adjunct assistant professor at UT Southwestern. Known affectionately as Dr. Andy, he has spent his career addressing the complex emotional and psychological factors behind pediatric eating disorders. Dr. Andy emphasizes that these disorders are about much more than food, highlighting the emotional struggles and coping mechanisms that manifest through disordered eating and affecting individuals across all genders and races.

Dr. Andy’s commitment to the mission of Children’s Health to “make life better for children” is evident through his involvement in fundraisers, donations, and community events like the Red Balloon Run & Ride. With a PhD in clinical psychology from The University of Texas Southwestern Medical Center and over two decades of experience in private practice, clinical teaching, and pediatric healthcare, Dr. Andy brings invaluable expertise and compassion to his work. Join us as he shares his insights into the intricacies of pediatric eating disorders and the importance of mental health care for young people.
In high school and college, I never really knew what I wanted to do. Then, there was a point where I went to a therapist and realized that something that I really value is mental health, so I decided to go back to school and pursue it. The eating disorder focus came along because I was working at a private school, and my boss asked me to speak at a symposium organization called The Elisa Project. It is no longer called the Elisa Project but the National Eating Disorder Association now. So, anyway, I spoke and had no idea what I was talking about because eating disorders were something new to me since everything was very new to me in my career in psychology. From that point, it grew on me, and I started getting involved with the Elisa Project and working at Children’s in the summers. When I wasn’t working at the schools, I would be at the hospital. One of the first groups I ever ran was a group of girls that dealt with eating disorders. Ever since that, for the last 12 years, I have been working here at Childrens in Plano, where they have an eating disorder program for patients who struggle with eating disorders.
The most common diagnoses of eating disorders that we see here at Children’s are Anorexia Nervosa and Bulimia Nervosa. We also have an outpatient program for kids who are diagnosed with Avoidant Restrictive Food Intake Disorder (ARFID), which is different from anorexia and bulimia since the primary concerns are not about body image and weight, shape, or appearance. At diagnosis, we learn that some kids have had some experience with choking or some type of trauma that has made them afraid to eat, not because of fears about gaining weight, but because they’re they’re afraid to that they might choke, or they might vomit, or they might have stomach pain, those kinds of things. The similarities that they share are anxiety, depression, or trauma. And so we treat adolescents and children since eating disorders are most commonly developed post-puberty, but we are also aware that adults can also develop eating disorders in adulthood.
I think parents should be aware of mental health problems and look out for any concerns that may develop into bigger problems. They should pay attention to how people around their children express themselves about appearance, body shape, or even how they talk about food. That way, they are aware of the message their daughter or son is receiving. It’s important to also always remind your child at an early age what self-love is and how it looks. As parents or caregivers, we must prepare them mentally because society can be cruel, and sometimes the message society gives us is not always right. We have to be mindful that as technology advances, things like social media, TV, and magazines can have a big influence on our children. Nowadays, that potentially puts our new generation of children at higher risk of developing mental health problems.
I also think sharing awareness is everything. There are so many people who have no idea how severe an eating disorder is or what it even is. For example, most of our kids who develop an eating disorder were suggested by a healthcare professional to lose weight. It may not develop into a full-blown eating disorder. Still, they may start doing things like restricting the food they intake or start developing a feeling of guilt when they eat, which may potentially develop an eating disorder. This is why I state that it’s important how we, as caregivers, relay the message in the best way to our patients or children.
Here at Children’s, we offer both inpatient and outpatient treatment. The inpatient program is typically offered to patients with severe health conditions due to the damage that eating disorders cause. Our nurses focus on getting the inpatients better and taking them out of that risk zone so they can be at home.
The outpatient program is offered to patients who are in a better state of health or who have gotten better and are no longer at risk. We also offer daily therapy activities like music therapy, art therapy, reading therapy, and just any fun activities our patients request to get their minds off of any negative thoughts they may encounter while in recovery. The Children’s Eating Disorder unit provides our patients with individual and family therapy and also gives the parents the resources they need even after the patient graduates the recovery program. We do our best to equip our families with whatever they need.

Oh boy, I wish there was a great answer. We still hear things that happen at schools that are not helpful. For example, some schools have curriculums that have things that emphasize weight loss, which can create more body shaming. The key is education in all communities. I’ve seen people who have no resources and live in poverty have eating disorders, and I have also seen people with all the resources in the world have it even worse.
People in underserved communities may have a harder time getting as much information about eating disorders, and then they have all the other obstacles. Sometimes we have food-insecure families. Food insecurity is associated with eating disorder behaviors anyway. All those kinds go with what we call the social determinants of health, you know, which include food insecurity, transportation, security, all those things just make life more complicated than it is. I believe that raising awareness in our communities may be exemplified by initiatives like Dallas Doing Good. To those in our community who are unaware of eating disorders, we should all raise awareness of them.
Several years ago, a kid came into the hospital and was in a wheelchair because he was severely underweight. At that point with anorexia, you can’t afford to really burn any more calories, it’s not safe to be moving around. And so I’m talking to this kid, and he said he needed to lose more weight. To everybody else in the world, you would have thought, “You are so severely underweight,” which this kid was– but the kid couldn’t see it. You know, as it is with eating disorders, you have some distorted kind of views about yourself. It makes you think that you’re overweight, and you lose more weight, which is really dangerous because, in a situation like that, this kid could have died.
But that kid had a long treatment because they had to be in the hospital for quite a while because he needed to restore a lot of weight. But, you know, he did recover. A lot of that happened here. He recovered and graduated from high school, and is now a college student. I think he is interested in mental health as well, and has done some really cool advocacy things to help others, too. Some kids don’t think they will make it to age 18. They think they won’t survive, but to see them graduate from high school, and go to college… it’s pretty amazing.
I’m so glad Dallas Doing Good is raising awareness about this. Even in mental health awareness month, people don’t think about eating disorders. They think about depression, anxiety, and all those things that commonly go along with eating disorders, but not the food aspect.
If you or someone you know are encountering eating disorder behaviors or dealing with an eating disorder, I recommend looking up our website, where we have all the contact information. I also recommend consulting with your primary physician and telling them about any concerns or questions you may have. Since technology has advanced so much, it is also easier to access resources or information that may come in handy.
Sign up with your email address to receive good stories, events, and volunteer opportunities in your inbox.